India’s efforts to fight antibiotic resistance GS: 3 :EMPOWER IAS
India’s efforts to fight antibiotic resistance
In news:
- The evolution of dietary, widespread use of antibiotics and hygienic habits in Western countries is associated with a decrease in the bacteria that help in digestion.
- These very bacteria were also found in the Iceman, who lived 5300 years ago, and are still present in non-Westernized populations in various parts of the world.
What is an antibiotic?
- Antibiotics, also known as antimicrobial drugs, are drugs that fight infections caused by bacteria in both humans and animals.
- Antibiotics fight these infections either by killing the bacteria or making it difficult for the bacteria to grow and multiply.
- Antibiotics only treat certain bacterial infections. Antibiotics do not have any effect on viruses.
Facts related to Antibiotics:
- Antibiotic resistance is one of the biggest threats to global health, food security, and development today.
- Antibiotic resistance can affect anyone, of any age, in any country.
- Antibiotic resistance occurs naturally, but misuse of antibiotics in humans and animals is accelerating the process.
- A growing number of infections – such as pneumonia, tuberculosis, gonorrhoea, and salmonellosis – are becoming harder to treat as the antibiotics used to treat them become less effective.
- Antibiotic resistance leads to longer hospital stays, higher medical costs and increased mortality.
- A 2017 report commissioned by the Union Department of Biotechnology and the U.K. Research Council underlined that India had some of the highest antibiotic resistance rates among bacteria that commonly cause infections.
Antibiotic resistance:
- Antibiotic resistance occurs when bacteria develop the ability to defeat the drugs designed to kill them.
- Antibiotics are medicines used to prevent and treat bacterial infections.
- Antibiotic resistance occurs when bacteria change in response to the use of these medicines.
- These bacteria may infect humans and animals, and the infections they cause are harder to treat than those caused by non-resistant bacteria.
- Antibiotic resistance leads to higher medical costs, prolonged hospital stays, and increased mortality.
- It is a specific type of drug resistance.
- Antibiotic resistance evolves naturally via natural selection through random mutation, but it could also be engineered by applying an evolutionary stress on a population.
- Once such a gene is generated, bacteria can then transfer the genetic information in a horizontal fashion (between individuals) by plasmid exchange.
- If a bacterium carries several resistance genes, it is called multiresistant or, informally, a superbug.
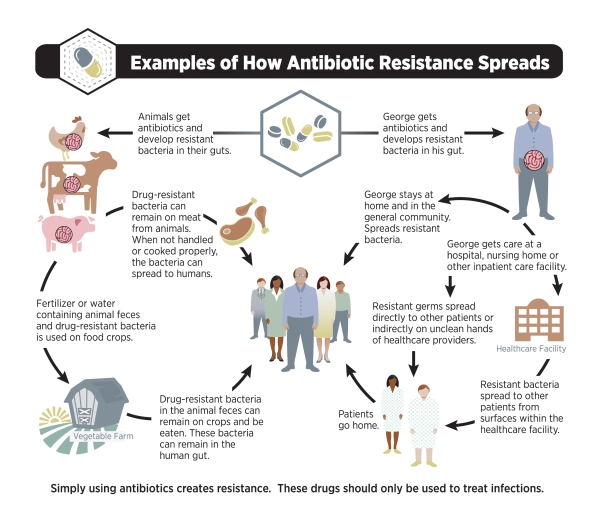
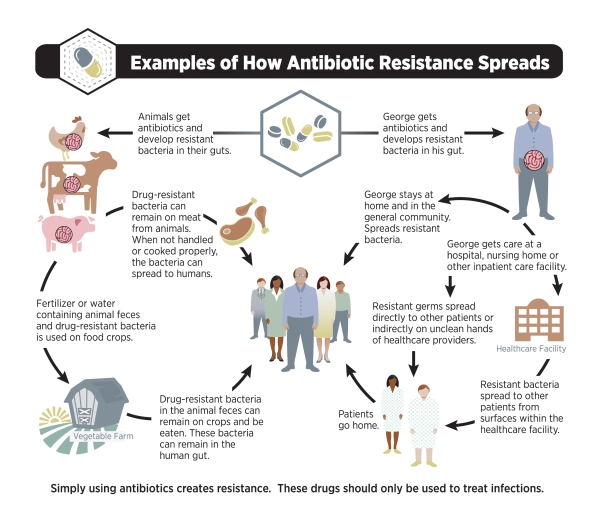
Transmission of antibiotics resistance:
Causes of antibiotic resistance:

Impact of antibiotic resistant:
- Antibiotic resistant bacteria can cause illnesses that were once easily treatable with antibiotics to become untreatable, leading to dangerous infections.
- Antibiotic-resistant bacteria are often more difficult to kill and more expensive to treat.
- In some cases, the antibiotic-resistant infections can lead to serious disability or even death.
- Antibiotic resistance is rising to dangerously high levels in all parts of the world.
- New resistance mechanisms are emerging and spreading globally, threatening our ability to treat common infectious diseases.
- A growing list of infections – such as pneumonia, tuberculosis, blood poisoning, gonorrhoea, and foodborne diseases – are becoming harder, and sometimes impossible, to treat as antibiotics become less effective.
- Organ transplantations, chemotherapy and surgeries such as caesarean sections become much more dangerous without effective antibiotics for the prevention and treatment of infections.
India’s efforts to fight resistance
- India first published almost nine years ago the broad contours of a plan to fight antimicrobial resistance.
- The difficulty has been in implementing it, given the twin challenges of antibiotic overuse and underuse.
- On the one hand, many Indians still die of diseases like sepsis and pneumonia because they don’t get the right drug at the right time.
- On the other hand, a poorly regulated pharmaceutical industry means that antibiotics are freely available to those who can afford them.
- The IACG report acknowledges these obstacles, and calls for efforts to overcome them.
Steps required
- Phasing out critical human-use antibiotics in the animal husbandry sector – Some steps can be initiated right away, it says, such as phasing out critical human-use antibiotics in the animal husbandry sector, such as quinolones.
- Multi-stakeholder approach -But these steps cannot be driven by regulation alone.A multi-stakeholder approach, involving private industry, philanthropic groups and citizen activists is needed.
- Responsibility of Private pharmaceutical – Private pharmaceutical industries must take it upon themselves to distribute drugs in a responsible manner.
- Responsibility of Philanthropic charities – Philanthropic charities must fund the development of new antibiotics, while citizen activists must drive awareness.
- These stakeholders must appreciate that the only way to postpone resistance is through improved hygiene and vaccinations.
Prevention and control
Antibiotic resistance is accelerated by the misuse and overuse of antibiotics, as well as poor infection prevention and control. Steps can be taken at all levels of society to reduce the impact and limit the spread of resistance.
- Individuals: To prevent and control the spread of antibiotic resistance, individuals can:
- Only use antibiotics when prescribed by a certified health professional.
- Never demand antibiotics if your health worker says you don’t need them.
- Always follow your health worker’s advice when using antibiotics.
- Never share or use leftover antibiotics.
- Prevent infections by regularly washing hands, preparing food hygienically, avoiding close contact with sick people, practising safer sex, and keeping vaccinations up to date.
- Prepare food hygienically, following the WHO Five Keys to Safer Food (keep clean, separate raw and cooked, cook thoroughly, keep food at safe temperatures, use safe water and raw materials)
- Policy makers :To prevent and control the spread of antibiotic resistance, policy makers can:
- Ensure a robust national action plan to tackle antibiotic resistance is in place.
- Improve surveillance of antibiotic-resistant infections.
- Strengthen policies, programmes, and implementation of infection prevention and control measures.
- Regulate and promote the appropriate use and disposal of quality medicines.
- Make information available on the impact of antibiotic resistance.
- Health professionals: To prevent and control the spread of antibiotic resistance, health professionals can:
- Prevent infections by ensuring your hands, instruments, and environment are clean.
- Only prescribe and dispense antibiotics when they are needed, according to current guidelines.
- Report antibiotic-resistant infections to surveillance teams.
- Talk to your patients about how to take antibiotics correctly, antibiotic resistance and the dangers of misuse.
- Talk to your patients about preventing infections (for example, vaccination, hand washing, safer sex, and covering nose and mouth when sneezing).
- Healthcare industry: To prevent and control the spread of antibiotic resistance, the health industry can:
- Invest in research and development of new antibiotics, vaccines, diagnostics and other tools.
- Agriculture sector: To prevent and control the spread of antibiotic resistance, the agriculture sector can:
- Only give antibiotics to animals under veterinary supervision.
- Not use antibiotics for growth promotion or to prevent diseases in healthy animals.
- Vaccinate animals to reduce the need for antibiotics and use alternatives to antibiotics when available.
- Promote and apply good practices at all steps of production and processing of foods from animal and plant sources.
- Improve biosecurity on farms and prevent infections through improved hygiene and animal welfare.
WHO response
Tackling antibiotic resistance is a high priority for WHO. A global action plan on antimicrobial resistance, including antibiotic resistance, was endorsed at the World Health Assembly in May 2015. The global action plan aims to ensure prevention and treatment of infectious diseases with safe and effective medicines.
- The “Global action plan on antimicrobial resistance” has 5 strategic objectives:
- To improve awareness and understanding of antimicrobial resistance.
- To strengthen surveillance and research.
- To reduce the incidence of infection.
- To optimize the use of antimicrobial medicines.
- To ensure sustainable investment in countering antimicrobial resistance.
- The Global Antimicrobial Resistance Surveillance System (GLASS)
The WHO-supported system supports a standardized approach to the collection, analysis and sharing of data related to antimicrobial resistance at a global level to inform decision-making, drive local, national and regional action.
- Interagency Coordination Group on Antimicrobial Resistance (IACG)
The United Nations Secretary-General has established IACG to improve coordination between international organizations and to ensure effective global action against this threat to health security.
Source)
https://www.thehindu.com/todays-paper/tp-features/tp-sci-tech-and-agri/lifestyle-threat-to-gut-bacteria/article29748092.ece